Posted Invoices Overview
How to navigate the "Posted Invoices" section
This article is most relevant to billers or those who may be helping their organization with billing
Introduction
Posted invoices represent claims that have been successfully submitted. In this section, users can track the progress of claims, filter by payor, date range, or funding source, and group invoices for easier management.
The Posted Invoices page in Motivity provides a complete overview of all claims that are still open or not yet reconciled. It offers various tools to help you manage and follow up on claims efficiently.
Prerequisites
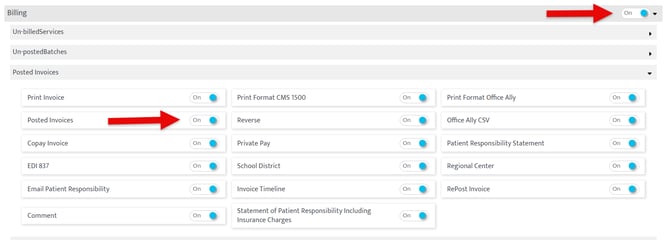
To use this feature, the access to the Billing Module must be turned on, as well as the "Posted Invoices" permission
How To Use
-Hover over the Motivity icon on top left corner and click on the billing menu to access this page 
-Then click the third category on the left called "Posted Invoices"

-You can also land on this page view by clicking on the ‘post’ button on Un-posted batches page

By default, the posted invoices page displays all open claims. To help manage these claims effectively, you can:
- Filter by Aging: This allows you to click on the related bucket to see claims listed by how long they’ve been open.
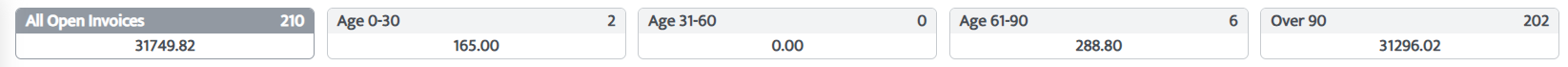
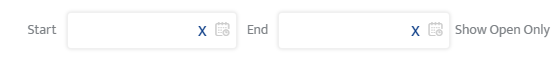
- Filter by Invoice Date: Use the date fields in the header to focus on claims within a specific time range.
- Search by Invoice Number: Use the search bar to find any specific claim you are looking for.
![]()
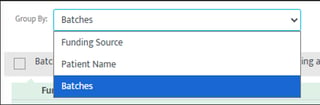
- Group by Funding Source or Patient or Batch: This option lets you see all claims for a patient, including both primary and secondary payors, or you can group by batches to view claims processed together or you can group by payor (funding source).
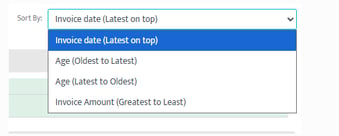
- Sort by Amount or Oldest Claims: You can also arrange claims by the biggest amounts or oldest pending claims to prioritize high-value or long-outstanding claims.
Motivity PM provides a handy green timeline icon next to each claim. This timeline shows the entire history of the claim, including:
![]()
- When the claim was generated.
- When it was posted.
- When it was sent to the payor.
- All subsequent statuses, including when the payment was received.
This gives you a full picture of the claim's lifecycle, making it easy to track its progress and identify where any delays may be occurring.
Claim Status Categories
To view the status of a claim
In Motivity, Accounts Receivable (AR) related to claims are organized into three primary buckets. Each bucket categorizes claims based on their current status in the billing process. These buckets help streamline the management of claims and identify the next steps for follow-up or action. Claims can move through various statuses during the billing process, from manual posting to submission through clearinghouses and payor review.
1. Clearinghouse
This bucket includes all claims that are currently with the clearinghouse, encompassing statuses related to submission and processing errors.
Statuses under Clearinghouse:
- Submitted to Clearinghouse: Claims that have been successfully submitted to the clearinghouse for processing.
- Clearinghouse File Acceptance Error: Claims that encountered file acceptance errors during submission.
- Clearinghouse File Configuration Error: Claims that had file configuration issues during the submission process.
- Rejected by Clearinghouse: Claims rejected by the clearinghouse that require correction or resubmission.
- Resubmitted to Clearinghouse: Claims that have been corrected and resubmitted to the clearinghouse.
- Regenerated & Resubmitted to Clearinghouse: Claims that have been updated and resubmitted to the clearinghouse for further processing.
2. With Payor
This bucket captures all claims that have been submitted to the payor and are either under review or awaiting a decision. It also includes claims that require further follow-up due to pending actions by the payor.
Statuses under Payor:
- Pending Response by Payor: Claims that are awaiting a response from the payor after submission.
- Under Review by Payor: Claims currently being reviewed by the payor.
- Rejected by Payor: Claims rejected by the payor, requiring correction, appeal, or resubmission.
- Reconciled – Balance to Secondary: Claims where the balance has been transferred to the secondary payor.
- Reconciled – Balance to Parent: Claims where the balance has been transferred to the parent payor.
3. Denials/Partial Payments
This bucket includes claims that have been denied by the payor or those that received partial payments. These claims require further action, such as denial management, appeals, or resubmission.
Statuses under Denials/Partial Payments:
- Claims Denied by Payor: Includes both fully denied and partially denied claims.
- Reconciled Partially: Claims that have been partially paid, but some balances remain unresolved.
Other Statuses
After organizing claims into the three primary AR buckets (Clearinghouse, With Payor, and Denials/Partial Payments), the remaining claim statuses fall outside of these categories, primarily relating to claims that have been resolved or are not actively part of the AR follow-up process. Here are the remaining statuses:
Posted (Non-Clearinghouse)
- Posted (Manual Posting): Claims that have been manually posted outside of the clearinghouse process and are not directly tied to the clearinghouse or payor follow-ups.
Patient Responsibility
- Emailed to Patient: Claims where patient responsibility has been identified, and the statement has been emailed to the patient for payment.
Reverted
- Voided (Reverted): Claims that have been voided.
Last Updated: 12/8/2025 by Blain Hockridge
