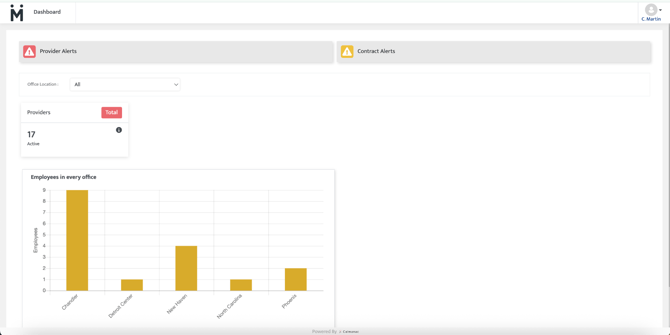
ConCred: Dashboard
ConCred dashboards provide high level alerts based on the contracts and providers in your organization. These alerts are intended to keep your organization in compliance with payor regulations.
Applies to ConCred users to provide an understanding of the alerts on the ConCred dashboard.
Dashboard Tiles
These tiles show you the key information pertaining to your role in ConCred.
The information you see is for the office location(s) you are assigned at the Admin level. Users can be assigned to one office, multiple offices or all offices depending on their role within the organization.

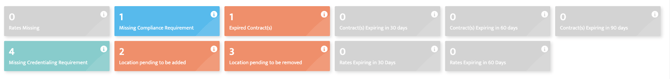
Re-Enrollment due
This tile shows you a list of total enrollments which have expired. This alert comes up if you have added a renewal date in the enrollment section.
Compliance: Pending information from provider
This tile shows you a list of total compliance items which are missing for the providers. Providers need to submit these items through the provider portal.
Compliance items include- certificates, degrees, licenses, training etc.
CAQH: ID is unavailable
This tile particularly shows you a count of providers who have not provided their CAQH ID to the credentialing team yet. This alert will only include providers who are required to have CAQH.
CAQH: Pending rostering
This tile shows you a count of providers who have provided CAQH IDs but they are not rostered under the organization's CAQH.
CAQH: Pending review
This tile shows you a count of providers who have added data on CAQH and attested it on CAQH but their data is not reviewed/pulled to ConCred yet.
Enrollments: Follow up due
This tile shows you a count of providers who have enrollment follow up alerts. This alert appears if a follow up date is set in the provider's enrollment page.
Compliance: Unverified credentials
This tile shows you a count of total compliance items which are submitted by the providers but which are not verified.
Compliance: Credentials expiring
This tile shows you a count of providers who have credentials or compliance items which are due for renewal in less than 60 days.
Compliance: Credentials expired
This tile shows you a count of providers whose compliance items have expired and need to be renewed.
Enrollments: Pending initial review
This tile shows a count of providers who have any ‘star marked’ enrollment requests, which are not in process or in network yet. This alert only considers enrollment requests who do not have any ‘missing requirements.
Enrollments: In initial review
This tile shows a count of providers who have any enrollments in the state- “Initial Review”.
Enrollments: Prover Review Pending (Over 10 Days since assignment)
This tile shows a count of providers who have not turned in their Enrollment application requested by the credentialing department/team to them for over 10 days.
Enrollments: Final Review Pending
This tile shows a count of providers who have submitted their enrollment application for final review to the credentialing team and credentialing department/team has not submitted the application to the payor by marking it as submitted.
Enrollments: Approval Pending (over 30 days since submission)
This tile shows a count of providers for whom enrollment application has been sent and the approval is not received for over 30 days.
Enrollments: Approval Pending (over 60 days since submission)
This tile shows a count of providers for whom enrollment application has been sent and the approval is not received for over 60 days.
Enrollments: Approval Pending (over 120 days since submission)
This tile shows a count of providers for whom enrollment application has been sent and the approval is not received for over 120 days.
Compliance: Over Due (Passed grade period)
This shows a count of providers for whom the due date for any compliance item(s) has passed.
Compliance: On Grace Period
This shows a count of providers who require certain compliance items to meet requirements within the set ‘grace period’.
Alerts Section
This section lists all the alerts pertaining to providers you are in charge of.
You can filter the alerts by selecting from alerts dropdown.
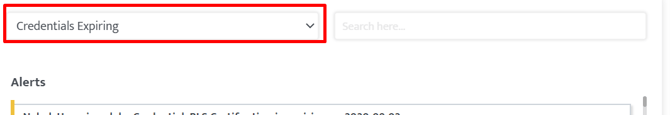
You can search for any specific provider by typing their name in the search bar.
These alerts will be removed automatically when the corresponding criteria is fulfilled.
Notifications Section
This section lists all the notifications pertaining to providers you are in charge of. The difference between an alert and a notification is that notifications are more for your information about any important updates and do not call for any action.
Types of notifications
Provider added
When a new provider is added to your location and their provider portal is created.
Provider terminated
When a provider is terminated from your location
New contract is added
When a new contract is added in the system.
New location is added
When a new location is added in the system.
Note is added by the provider
When a note is added by a provider on the enrollment page.
New enrollment requested
When an enrollment request is added to the queue by ‘star marking’ the enrollment for any location/payor.
Note is added by the provider
A new note is added by the provider for any compliance item or enrollment.
Note is added by credentialing team member
A new note is added by the provider for any compliance item or enrollment.
Credentialing team member is assigned
Credentialing team members are assigned to handle action items for any provider.
Assigned to
This filter on top is access based. Through the correct selection you can see the alerts assigned to the providers to you vs alerts assigned to the providers to some other team members vs all the alerts in the system.
Last Updated: 12/8/25 by Maggie Yost
