ConCred: Providers List
In this article you will learn how to access providers and add a new provider, including assigning a provider to their service locations in ConCred.
This article is for ConCred users who add and manage providers in Motivity.
To access providers, hover over the ConCred icon on the top left corner to access your menu and click on the providers menu to access your list of all providers.
Filters
On the providers list page, by default you will see a list of all the providers who you have access to.
You can also filter providers by office, title, or who they are assigned to:
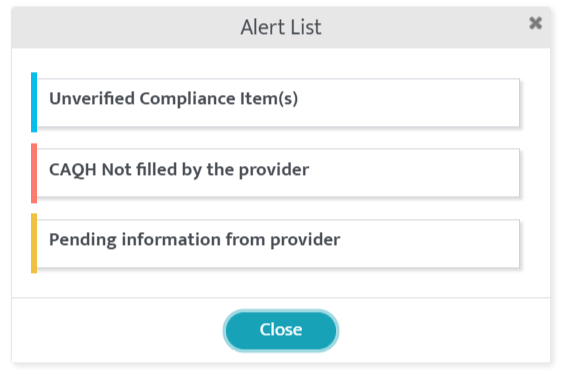
You can click on the ‘alert’ icon to see a quick list of all the alerts within provider’s profile.
![]()
Example:
Add a new Provider
Use the button on the top right corner of this page to add a new provider.
You have to fill at least the mandatory fields on the ‘Provider Basic Info’ page to create a new provider, as indicated by a red asterisk.
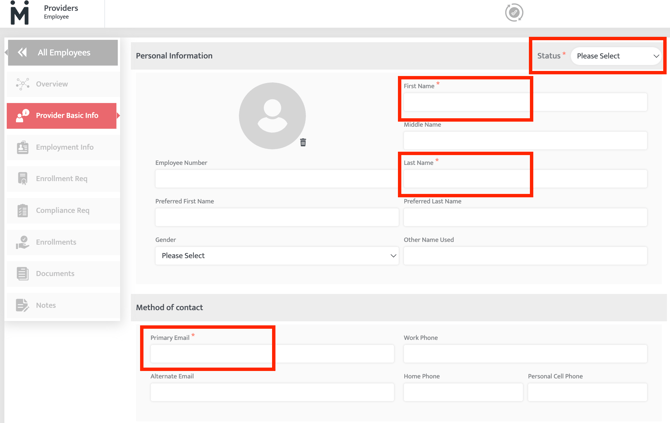
Once the ‘Provider Basic Info’ is filled, your other menu on the page will be unlocked.
Provider Portal Account Creation and Access
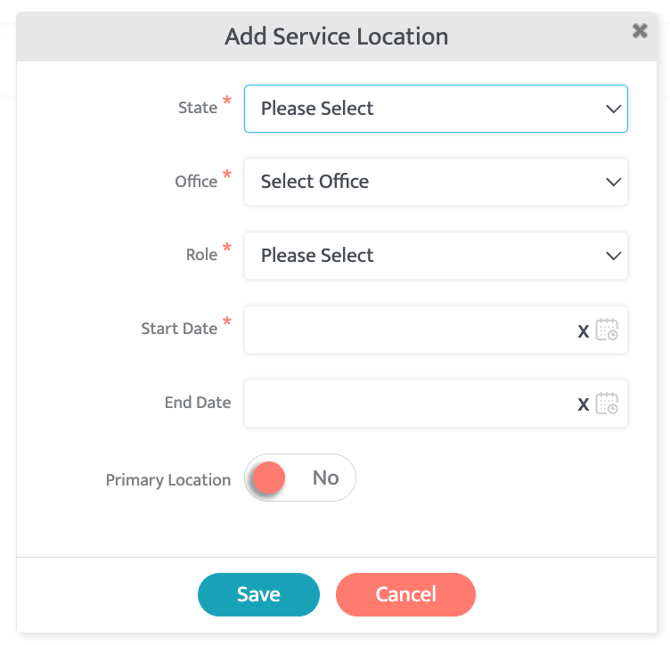
After addition of the ‘Provider Basic Info’, the next step is to add ‘Employment Info’ of the provider. A Provider Portal account will be created for the provider when at least one service location is added under ‘Employment Info’. Providers will get an email invite to access their provider portal account.
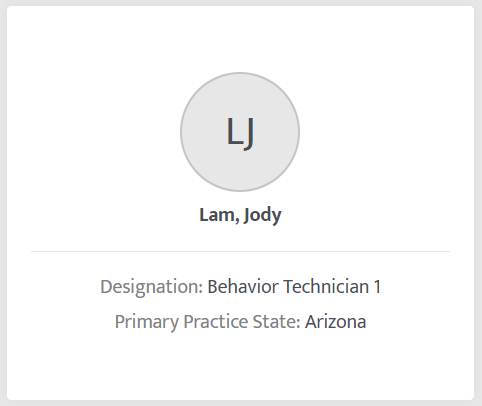
Provider Info Tile
This tile reflects the profile picture, name of the provider, their designation and their primary service location.
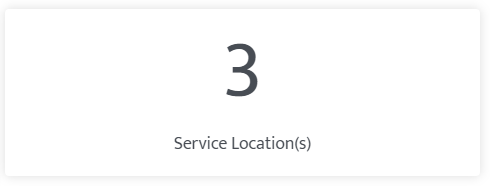
Service Location(s)
This tile will show a count of service locations where the provider is providing services. Clicking on this tile will take you to the ‘Employment Info’ menu from the left panel where you can see a list of all their service locations and roles at each location.
Pending Requirements
This tile shows you a status of any pending requirements for any current or upcoming Enrollments for the provider.
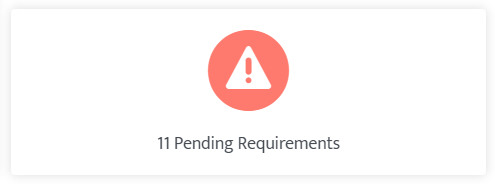
Clicking on this tile will take you to the ‘Enrollment Req’ menu from the left panel where you can see a list of all compliance items needed by the organization or by the payors for the required Enrollments.
If there are no pending requirements then you will see a check mark showing you that the provider has submitted all required compliance items.
Note:
If you see the pending requirements alert but on ‘Enrollment Req’ page you don’t see any pending items then be sure to check the compliance requirement menu.
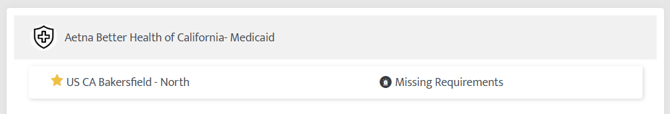
Enrollment Request
Ideally a provider should be Enrolled with all the payors at their service location so that they can work on any case at any time however considering the tedious process of Enrollment and limited resources at credentialing department, you can choose to enroll providers only under specific payors. In this case generally (operations) manager/credentialing team is required to submit specific Enrollment requests for the providers.
Click on the ‘Add Enrollment Request(s)’ button to navigate to the Enrollments page where you can add requests to the queue.
![]()
Enrollments
This section will show a list of all the Pending, In-Progress or Completed Enrollments.
If no Enrollments are requested for any provider, then you will see this message-
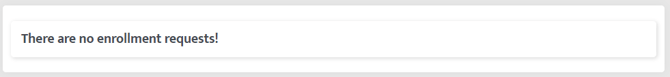
Clicking on the payor name will take you to the Enrollment Details page where you can see statuses along with action items (if any).
NEW ARTICLE- ConCred: Provider Alerts
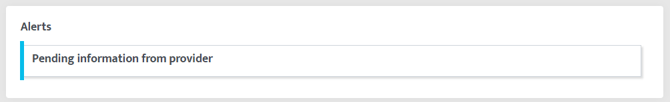
Alerts
This section will highlight all the alerts which require your attention. These alerts will go away when the provider takes the required action.
Example:
Here are the types of alerts you will see, and how they will be removed-
Alert: Re-enrollment due in less than 60 days
Relevant Page: Enrollment
Reason: This alert comes up if you have added a renewal date in the enrollment section and it is reaching in less than 60 days. This alert will be automatically removed if a new future approval date is added or if it is marked as ‘not being added’ or if enrollment crosses expiry date. After the expiry date the alert moves to the “Enrollment Expired” category.
Alert: Enrollment expired
Relevant Page: Enrollment
Reason: This alert comes up if you have added a renewal date in the enrollment section and it has passed the renewal date. This alert will be automatically removed if a new future approval date is added or if it is marked as ‘not being added’.
Alert: Pending information from provider
Relevant Pages: Enrollment Req, Compliance Req
Reason: Provider has missing information in Enrollment Req or Compliance Req tabs. Once the provider adds/uploads all the missing information or this item is marked as ‘Not being added’ then this alert will be removed automatically.
Alert: CAQH ID is unavailable
Relevant Page: Enrollment Req (Only for roles which require CAQH based on contract’s compliance requirements)
Reason: The provider has not given their CAQH ID yet. Once the provider adds CAQH details then this alert will be removed automatically.
Alert: Pending CAQH rostering
Relevant Page: CAQH (Only for roles which require CAQH based on contract’s compliance requirements)
Reason: Provider has given CAQH IDs but they are not rostered under organization’s CAQH. Once a provider is added under the organization’s CAQH account then this alert will be removed automatically.
Alert: Pending CAQH review
Relevant Page: CAQH (Only for roles which require CAQH based on contract’s compliance requirements)
Reason: Provider has added data on CAQH and attested it on CAQH but their data is not reviewed/pulled to ConCred yet. If CAQH data is pulled into ConCred then this alert will be removed automatically.
Alert: Enrollment follow up due
Relevant Page: Enrollment
Reason: This alert appears on the follow up date set in the provider's enrollment page. This will be removed when the follow up reminder is dismissed.
Alert: Unverified compliance item(s)
Relevant Pages: Enrollment Req, Compliance Req
Reason: The provider has submitted the details but they are in ‘unverified state’. Once you verify it, this alert will be automatically removed.
Alert: Credentials expiring
Relevant Pages: Enrollment Req, Compliance Req
Reason: Provider has one or more compliance items which require renewal in 60 days or less. Once the provider adds the renewed details or this item is marked as ‘Not being added’ or when the expiry date is crossed then this alert will be removed automatically.
Alert: Credentials expired
Relevant Pages: Enrollment Req, Compliance Req
Reason: Provider’s one or more compliance items have expired. Once the provider adds the renewed details or this item is marked as ‘Not being added’ then this alert will be removed automatically.
Alert: Enrollments: Pending initial review
Relevant Page: Enrollment Details
Reason: Enrollment is ‘star marked’ hence it is in enrollment requests queue and it does not have any ‘missing requirements’. This alert will be removed once status of enrollment changes to ‘Initial Review’ or any further step in the workflow.
Alert: Enrollments: In initial review
Relevant Page: Enrollment Details
Reason: Enrollment application has been generated. This alert will be removed once the application is either assigned to the provider for further review or submitted to the payor or if the workflow is abandoned.
Alert: Enrollments: Provider review pending
Relevant Page: Enrollment Details
Reason: Enrollment form is assigned to the provider by the credentialing team. Once they submit the application back the status will change to ‘Pending Final Review’ and this alert will be removed automatically. This alert will be also dropped if the workflow is abandoned.
Alert: Enrollments: Final review pending
Relevant Page: Enrollment Details
Reason: Provider has submitted their enrollment application for final review to the credentialing team. This alert will be removed automatically when the application is moved to “Submitted” (to payor) stage or if the workflow is abandoned.
Alert: Enrollments: Approval pending (over 30 days since submission)
Relevant Page: Enrollment Details
Reason: Enrollment application has been submitted to the payor but the approval is not received yet. This alert will be removed automatically when the approval date is added or if over 60 days have passed since submission or if the workflow is abandoned.
Alert: Enrollments: Approval pending (over 60 days since submission)
Relevant Page: Enrollment Details
Reason: Enrollment application has been submitted to the payor but the approval is not received yet. This alert will be removed automatically when the approval date is added or if over 120 days have passed since submission or if the workflow is abandoned.
Alert: Enrollments: Approval pending (over 120 days since submission)
Relevant Page: Enrollment Details
Reason: Enrollment application has been submitted to the payor but the approval is not received yet. This alert will be removed automatically when the approval date is added or if the workflow is abandoned.
Alert: Compliance: Over due (passed grace period)
Relevant Pages: Enrollment Req, Compliance Req
Reason: Due date for any compliance item(s) has passed based on grace period (refer 10.3.11) set in the contract. Once the provider adds/uploads the missing information or this item is marked as ‘Not being added’ then this alert will be removed automatically.
Alert: Compliance: On grace period
Relevant Pages: Enrollment Req, Compliance Req
Reason: Provider has missing information in Enrollment Req tab which is on grace period set in the contract. Once the provider adds/uploads the missing information or this item is marked as ‘Not being added’ then this alert will be removed automatically.
Notifications
This section will list down important activities. However, it does not require any action from you.
Example:
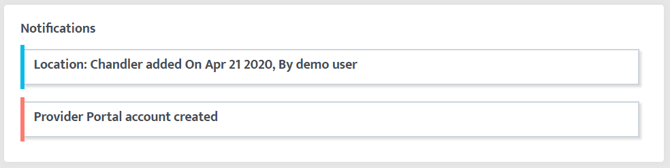
Here are the types of notifications you will see-
Provider added
New location added
New enrollment requested
Enrollment status changed
Provider terminated
New contract added (potentially applicable to this provider)
Note is added by the provider
Note is added by credentialing team member
Credentialing team member is assigned
Last Updated: 12/8/25 by Maggie Yost
