Understanding Compliance Alerts & Updates in Motivity Scheduler
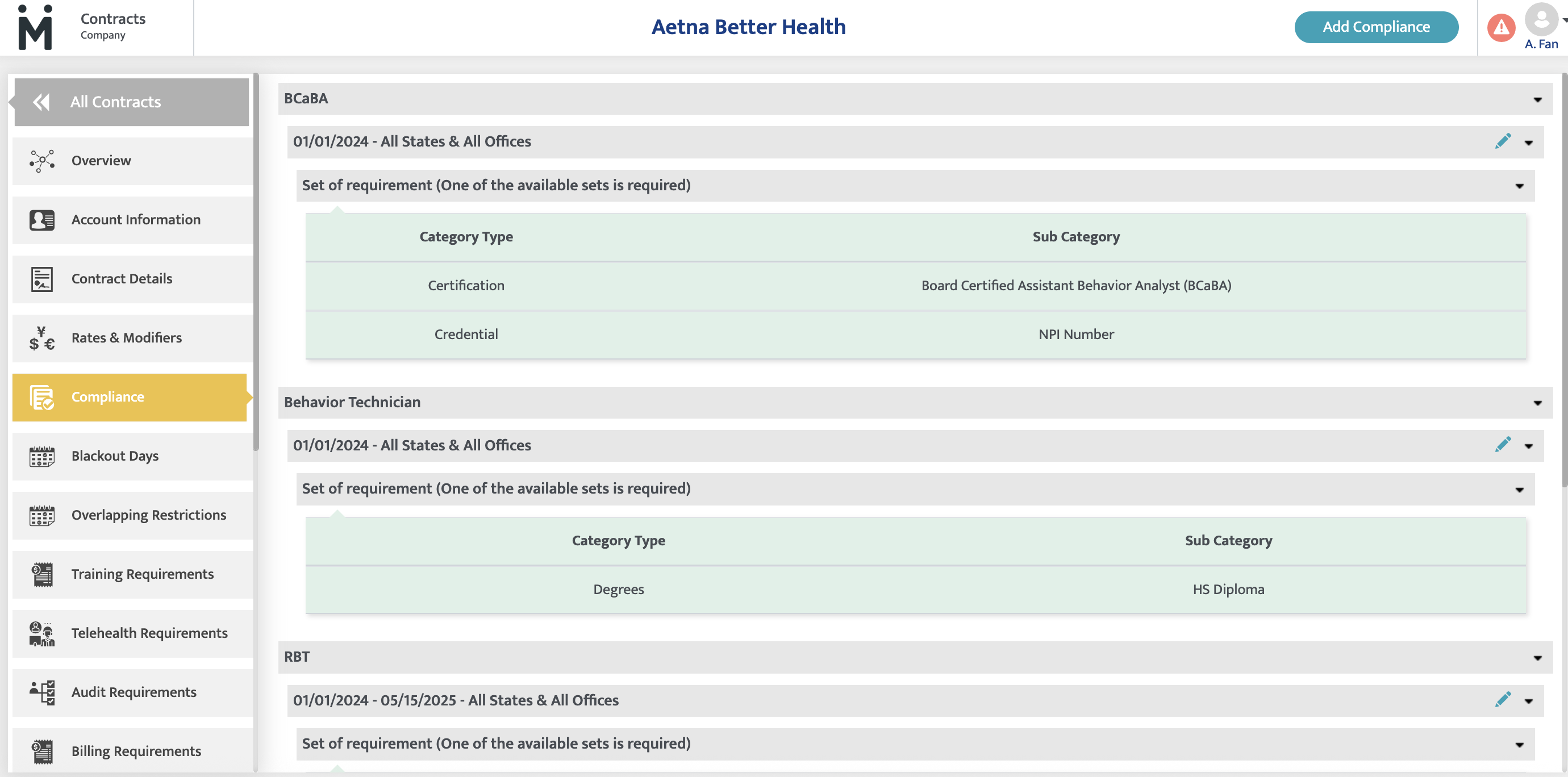
Compliance alerts in Practice Management appear when an appointment does not meet the necessary compliance criteria. These checks ensure that providers meet organizational, payor, and regulatory requirements before scheduling services.
Key Reasons for Compliance Alerts:
- The provider lacks the required credentials, certifications, or training.
- The provider’s compliance items (e.g., background checks, CPR certification) are missing, expired, or unverified.
- The location or service has additional compliance requirements that the provider does not fulfill.
Importance of Compliance Alerts
- Helps prevent scheduling conflicts with non-compliant providers.
- Ensures all scheduled appointments meet industry and payor requirements.
- Reduces billing rejections and compliance risks.
- Immediate Updates: Changes to patient funding sources and authorization details show up instantly.
- Within 15 Minutes: Updates to provider compliance records (e.g., added certifications) take effect quickly.
- Overnight Updates: Major changes, such as contract updates, role clearance rules, and provider enrollment changes, update the next day.
Common Mistakes & How to Avoid Them
- Expecting instant alert removal – Some updates require processing time.
- Confusing enrollment updates with compliance updates – Enrollment changes may take longer to reflect.
- Overlooking contract-specific compliance rules – Some rules are tied to contracts and need overnight processing.
Checklist for common mistakes
1. Review the Contracts Location: Contracts-Account Information-Service Locations

3. Review provider location setup: Provider Module- Employment Info

4. Review the provider compliance setup to ensure it is up to date and meets the payer’s requirements. Refer to the Provider Module under "Enrollment Requirements" and "Compliance Requirements.

5. Review provider enrollment: Provider Module- Enrollments.
*if you are not seeing the payer information when click "Add more", that's because if didn't complete the contract setup. You should go back to Contrcts module and complete contracts setup first.

